As COVID-19 continues to spread, many parents are on high alert about fevers in their children. Fevers often accompany the array of viral illnesses that peak during cold and flu season. With COVID-19 in circulation, a fever may signal this rather than a typical seasonal virus. This guide arms parents with information to respond appropriately when your child spikes a temperature during this pandemic.
What’s Considered a Fever in Children?

A fever indicates a higher-than-normal body temperature. Fevers are one of the immune system’s responses to fighting off infection.
In children, a fever is technically defined as:
- Babies under 3 months: rectal temperature above 100.4°F (38°C)
- Children 3-36 months: temperature above 100.4°F (38°C)
- Children 3 years and older: temperature above 101°F (38.3°C)
While a mild fever isn’t necessarily serious on its own, parents should monitor symptoms and check with a pediatrician. Fevers may also make children uncomfortable.
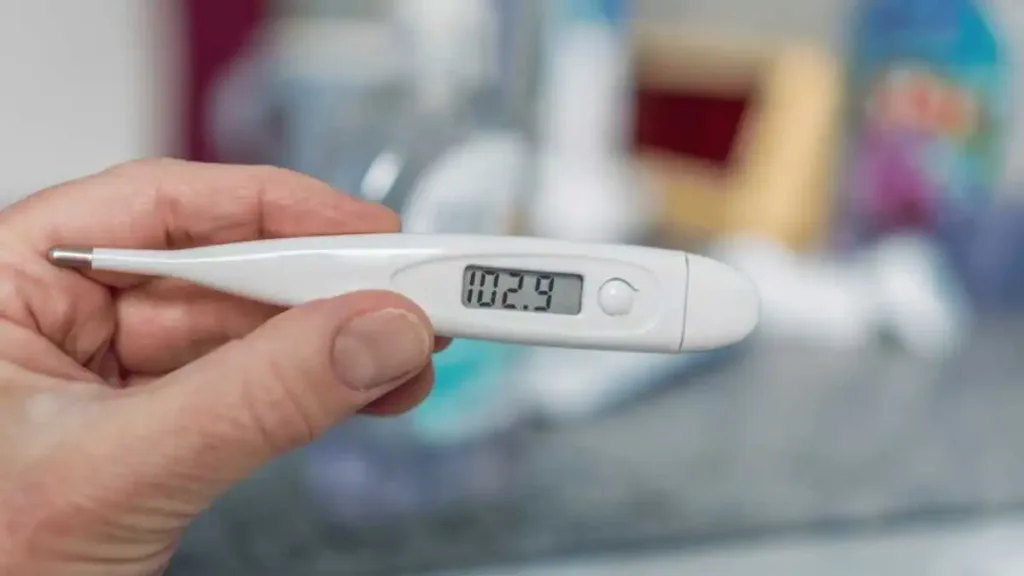
How to Check for Fever
Taking a child’s temperature rectally provides the most accurate reading for infants. For older children, temperature can be taken by mouth or with an ear, forehead, or armpit scanner thermometer.

Glass thermometers containing mercury should be avoided due to safety hazards if they break. Digital thermometers are faster and easier to use. Make sure to disinfect thermometers thoroughly after each use.
Proper methods for checking temperature:
Rectal
Lubricate the tip and gently insert no more than 1 inch into the rectum, holding for about one minute.
Oral
Place tip under the tongue towards the back of the mouth with lips closed for one minute.
Ear
Follow directions to gently place the thermometer probe snugly into the ear canal.
Forehead
Gently sweep across forehead avoiding hairline.
Armpit
Place under arm snugly and hold arm against body for one minute.
Take temperature at consistent times, such as morning and night. Tracking temperature helps identify patterns or spikes.
Possible Causes of Fever in Children
While all fevers stem from an underlying infection or inflammation, the specific causes vary.
Common culprits include:
- Viral infections like cold, flu, COVID-19, rubella, chickenpox, measles, mononucleosis.
- Bacterial infections such as strep throat, pneumonia, ear infection, urinary tract infection.
- Vaccine reactions – mild fever after vaccination is normal.
- Inflammatory conditions like arthritis, appendicitis, inflammatory bowel disease.
- Heat-related illnesses if body overheats and cannot cool properly.
- Teething in some babies once new teeth begin pushing through.
- Chronic conditions like cancer, autoimmune disorders, chronic fatigue syndrome.
During the COVID-19 pandemic, a new onset of fever is more likely to raise alarm for this virus. However, the spectrum of possible causes remains broad. Diagnostic testing can help determine whether COVID-19 or another condition is responsible.
COVID-19 Symptoms with Fever in Children
While infected children are less likely to become severely ill, COVID-19 is still a concern when fever crops up.

The CDC lists these COVID-19 symptoms that may accompany fever:
- Cough, sore throat, shortness of breath, difficulty breathing.
- Chills, muscle pain, headache, new loss of taste/smell.
- Congestion, runny nose, nausea, vomiting, diarrhea.
- Fatigue, lethargy, poor feeding or appetite in infants.
In a study of over 2,500 children with COVID-19, fever was the most common symptom, occurring in 56%. Cough was second most common at 54%. Other top symptoms were shortness of breath, diarrhea, muscle aches, and sore throat.
Not all COVID-19 cases clearly fit the typical symptom pattern. Many sick children exhibit only mild, non-specific symptoms. Monitoring for fever and any other changes is important.
When to Call the Pediatrician

Parents should contact their child’s pediatrician if:
- Fever in an infant under 3 months (a lower temperature threshold warrants attention).
- Temperature is over 104°F (40°C).
- Fever lasts more than 72 hours.
- Fever doesn’t respond to over-the-counter medications.
- Low-grade fever persists for over a week.
- Signs of dehydration arise – reduced urination, crying without tears, sunken eyes.
- Symptoms worsen or additional symptoms appear.
- Underlying chronic condition raises concerns about illness vulnerability.
- Confusion, stiff neck, difficulty breathing, inability to keep fluids down.
- Any symptom causes you major concern about your child’s well-being.
Severe or escalating symptoms may warrant visiting an emergency room versus a standard office visit. Otherwise, calling your pediatrician is an appropriate first step for evaluation and medical advice. Home treatment may be recommended, or an in-person visit scheduled if warranted.
COVID-19 Testing for Fever
The pediatrician will decide if a COVID-19 test is indicated based on the child’s profile of symptoms and fever.

Testing may be recommended if:
- Symptoms match the common COVID-19 pattern.
- No alternate clear diagnosis.
- High community COVID-19 transmission.
- Fever requires hospitalization.
- Child has risk factors like weak immune system.
PCR nasal/throat swab or saliva tests can diagnose active coronavirus infection. Turnaround times for results have improved in many regions. A positive test result confirms COVID-19 as the fever cause.
Treating Fever at Home
For mild to moderate fevers, home treatment may be appropriate if your pediatrician advises. Have the child rest, drink plenty of fluids, and dress lightly.

Key tips for managing fever at home:
- Use over-the-counter fever reducers like acetaminophen or ibuprofen; follow dosing directions carefully based on age/weight.
- Offer fluids regularly – water, diluted juice, ice pops, or electrolyte drinks to avoid dehydration.
- Cool with lukewarm sponge baths or washcloths to the forehead, neck and wrists.
- Dress in light, breathable clothing and cover with a light blanket.
- Provide cold treats like ice pops and Italian ice to soothe sore throats.
- Keep room temperature comfortably cool and child well-rested.
- Avoid decongestants and cough/cold medications without doctor approval.
Closely monitor symptoms and alert your doctor if the fever persists beyond 3 days or worsens despite treatment. Your pediatrician can reassess if home care remains adequate.
Precautions to Avoid Spreading Illness

If your child has a fever, take measures to avoid the spread of any contagious illness:
- Follow isolation guidelines if COVID-19 is confirmed – usually 10 days after symptom onset and 24 hours fever-free without medication.
- For flu, strep throat, or other contagious conditions, follow your doctor’s guidance on isolation.
- Everyone in close contact should practice diligent hand washing and avoid touching their face.
- All family members should wear well-fitted masks at home, especially when unable to distance.
- Disinfect high-touch surfaces, toys, doorknobs, bathrooms regularly.
- Avoid contact with vulnerable individuals like elderly relatives or those with weakened immune systems.
- Keep your child home from school/daycare until the fever resolves and your pediatrician determines it’s safe to return.
Following public health guidelines for isolation and sanitization helps contain the spread of illness through communities.
When to Visit the Emergency Room

In more severe cases, fevers may warrant emergency care. Rush your child to the ER if they exhibit:
- Very high temperature above 104°F (40°C) that does not improve with medication.
- Signs of respiratory distress – fast breathing, nostrils flaring, ribs pulling in with each breath.
- Blue-tinged lips, mouth, fingers – indicator of low oxygen.
- Altered mental state – disorientation, lethargy, inability to wake.
- Seizures or convulsions.
- Dehydration with little urination – sunken eyes, lack of tears, dry mouth, dizziness.
- Fever in a newborn under 2 months – higher risk of serious complications.
- Any symptom causing major alarm about your child’s well-being.
Severe symptoms suggest the body is losing its battle against infection and may lead to dangerous complications. Prompt ER intervention can provide life-saving treatment and enable a full recovery.
Monitor Fever Carefully but Avoid Panic
Fevers are common in childhood due to routine infections. While concerning, parents can usually manage mild fevers safely at home with pediatrician guidance. Monitoring symptoms, maintaining hydration, and using antipyretic medications helps.
However, fevers require more vigilance during the COVID-19 pandemic given this virus’ presence in communities. Check in with your pediatrician for direction on managing fever, indications for testing, and appropriate isolation.
Pay close attention for worsening symptoms or signs of distress. Follow public health protective measures to avoid disease spread. With proactive care and your doctor’s input, your child can rest, recover and return to fever-free health.
Frequently Asked Questions
How long can a fever last in children before becoming a concern?
Fevers generally last 2-3 days but up to 5 days can be normal for viral illnesses. However, contact your pediatrician if a fever persists over 3 days without improvement or other symptoms worsen.
What temperature is considered a low-grade fever versus a high fever in children?
Low-grade fevers range from 100-102°F. Moderate grade fevers are 102-104°F. High fevers are over 104°F. Temperatures above 104°F warrant closer monitoring and medical care.
Should I give my child medicine to reduce any fever?
Medications like acetaminophen or ibuprofen can provide relief from discomfort and bring temperatures down. Follow pediatrician advice on proper dosage and timing based on your child’s age.
How can I tell if my child is dehydrated when they have a fever?
Signs of dehydration include reduced urination, sunken eyes, crying without tears, parched lips, dizziness. Offer plenty of fluids and contact your pediatrician if you notice these red flags.
Is it harmful for fevers to get too high in children?
Very high uncontrolled fevers over 104°F can induce seizures or breathing trouble. Medications and lukewarm baths help lower dangerous high temperatures. Immediately contact your pediatrician or ER.
When is a COVID-19 test appropriate for a child with fever?
COVID-19 testing may be warranted if fever symptoms match the common pattern and have no clear alternate diagnosis. Your pediatrician makes this determination during consultation.
Can I give my child over-the-counter cold medicines when they have a fever?
Avoid decongestants and multi-symptom cold medicines without your pediatrician’s approval. They are generally not recommended for young children.
Is it safe to send my child back to school after their fever is gone?
They can return once fever-free for 24 hours without medication. Follow your pediatrician and school’s guidance on when resuming normal activity is safe.
What foods help reduce fever in children?
No foods directly lower fever. Focus on fluid hydration. Soft, bland foods sometimes help with nausea. Avoid heavy, greasy foods which are harder to digest.

I’d like to find out more? I’d love to find out more details.
May I request that you elaborate on that? Your posts have been extremely helpful to me. Thank you!