I. Introduction

Definition of Human Microbiome
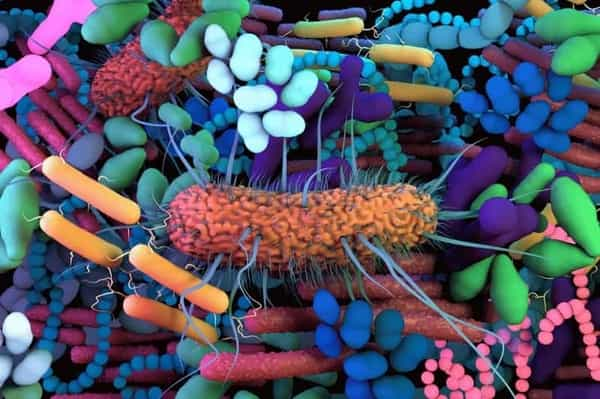
The human microbiome is defined as the collection of microorganisms, including bacteria, viruses, fungi, and other microbial species that live in and on the human body. These microorganisms interact with each other, as well as with their human host, in complex ways that play a vital role in human health and disease.
The human microbiome is found in various parts of the human body, such as the skin, mouth, gut, and genital tract. These microbiomes vary in composition and diversity depending on the body site, lifestyle, and other factors such as age, diet, and genetics.
The human microbiome is essential for the development and regulation of the immune system, digestion and absorption of food, and protection against pathogens. It produces a range of metabolites, including vitamins, hormones, and neurotransmitters, that influence various physiological processes in the body.
Recent advances in sequencing technology have allowed scientists to study the human microbiome in more detail, revealing the incredible diversity and complexity of these microbial communities. However, there is still much to be learned about the human microbiome, and ongoing research in this field holds great promise for the development of novel therapeutic approaches for a range of diseases.
Importance of Human Microbiome
The human microbiome plays a crucial role in human health and disease, and its importance cannot be overstated.
Here are some key reasons why the human microbiome is so important:
Protection against pathogens: The microbiome is a barrier against harmful pathogens by preventing them from colonizing and infecting the host. This protective function is particularly important in areas such as the gut and skin, where pathogens are most likely to enter the body.
Regulation of the immune system: The microbiome plays a critical role in the development and regulation of the immune system, which is responsible for protecting the body against infections and other foreign invaders. A healthy microbiome helps to train the immune system to recognize and respond appropriately to different types of pathogens, while also preventing the immune system from overreacting and causing damage to the host.
Digestion and absorption of food: The microbiome helps to break down and digest complex carbohydrates, fiber, and other components of our diet that the human body is unable to digest on its own. This process not only provides us with important nutrients but also helps to maintain a healthy balance of bacteria in the gut.
Production of metabolites: The human microbiome produces a range of metabolites, including vitamins, hormones, and neurotransmitters, that have a wide range of physiological effects on the host. For example, the gut microbiome is involved in the production of serotonin, a neurotransmitter that plays a key role in regulating mood, appetite, and sleep.
Influence on disease: The microbiome has been linked to a growing number of diseases, including inflammatory bowel disease, obesity, diabetes, and even mental health disorders. Understanding the role of the microbiome in these diseases is an important area of research and holds great promise for the development of new therapeutic approaches.
The human microbiome is a complex and dynamic ecosystem that plays a critical role in human health and disease. Further research in this field will likely uncover even more important functions and potential therapeutic applications of the microbiome in the future.
Historical Background of Human Microbiome.
The history of human microbiome research dates back to the late 17th century when Antonie van Leeuwenhoek first observed microorganisms under a microscope. However, it wasn’t until the 20th century that scientists began to explore the microbiome in more detail.
In the early 1900s, Russian biologist Elie Metchnikoff hypothesized that the human gut microbiome played a crucial role in health and longevity. He proposed that consuming lactic acid bacteria, such as those found in fermented milk, could improve the health of the gut microbiome and extend the human lifespan. This theory laid the groundwork for the development of probiotics, which are now widely used to promote gut health.
In the mid-20th century, advances in microbiology and genetics allowed researchers to study the microbiome in greater detail. In 1972, microbiologist Joshua Lederberg introduced the term “microbiome” to describe the collective genetic material of microorganisms living in a particular environment, including the human body.
The advent of high-throughput sequencing in the 21st century revolutionized microbiome research by allowing scientists to identify and study the vast diversity of microorganisms present in the human microbiome. This led to the discovery of previously unknown microbial species and their roles in human health and disease.
Today, the study of the human microbiome is a rapidly growing field, with new discoveries being made all the time. The microbiome is now recognized as a key factor in human health and disease, and ongoing research in this area holds great promise for the development of new therapeutic approaches to a range of diseases.
Anatomy of Human Microbiome
What is Microbiome?
The human microbiome, in particular, is the collection of microorganisms that live in and on the human body. These microorganisms are found in various parts of the body, including the skin, mouth, gut, and genital tract.
The human microbiome is a complex ecosystem that interacts with its host in complex ways. It plays a vital role in many physiological processes, such as digestion and absorption of nutrients, regulation of the immune system, and protection against pathogens.
The composition and diversity of the human microbiome vary depending on the environment or host. For example, the microbiome of the gut is particularly diverse and contains a large number of bacterial species that help to break down and digest complex carbohydrates, fiber, and other components of our diet that the human body is unable to digest on its own.
Recent advances in sequencing technology have allowed scientists to study the microbiome in more detail, revealing the incredible diversity and complexity of these microbial communities. However, there is still much to be learned about the microbiome, and ongoing research in this field holds great promise for the development of novel therapeutic approaches for a range of diseases.
Different types of microorganisms present in the human microbiome
The human microbiome is a complex ecosystem that is home to a wide range of microorganisms, including bacteria, viruses, fungi, and other microbial species.
Here are some of the most common types of microorganisms found in the human microbiome:
Bacteria: Bacteria are the most abundant microorganisms in the human microbiome, and they play a vital role in human health and disease. They are found in various parts of the body, including the skin, mouth, gut, and genital tract, and they help to break down and digest complex carbohydrates, fiber, and other components of our diet that the human body is unable to digest on its own.
Viruses: While less common than bacteria in the human microbiome, viruses play an important role in shaping the composition and function of the microbiome. They can infect and kill bacteria, influencing the balance of microbial species in the human microbiome.
Fungi: Fungi are also found in the human microbiome and can have both beneficial and harmful effects on human health. For example, some species of fungi help to break down complex carbohydrates in the gut, while others can cause infections in immunocompromised individuals.
Archaea: Archaea are a group of microorganisms that are similar to bacteria but have different cell structures and genetic makeup. They are found in low numbers in the human microbiome and are thought to play a role in the metabolism of certain compounds in the gut.
Protists: Protists are a diverse group of microorganisms that include single-celled organisms such as amoebas and algae. They are found in low numbers in the human microbiome and are thought to play a role in regulating the immune system.
Helminths: Helminths are parasitic worms that live in the gut and can have both beneficial and harmful effects on human health. Some species of helminths have been shown to regulate the immune system and reduce inflammation, while others can cause disease.
Understanding the different types of microorganisms present in the human microbiome and their interactions with the host is a critical area of research, with potential implications for the development of new therapeutic approaches for a range of diseases.
How Human Microbiome Develops
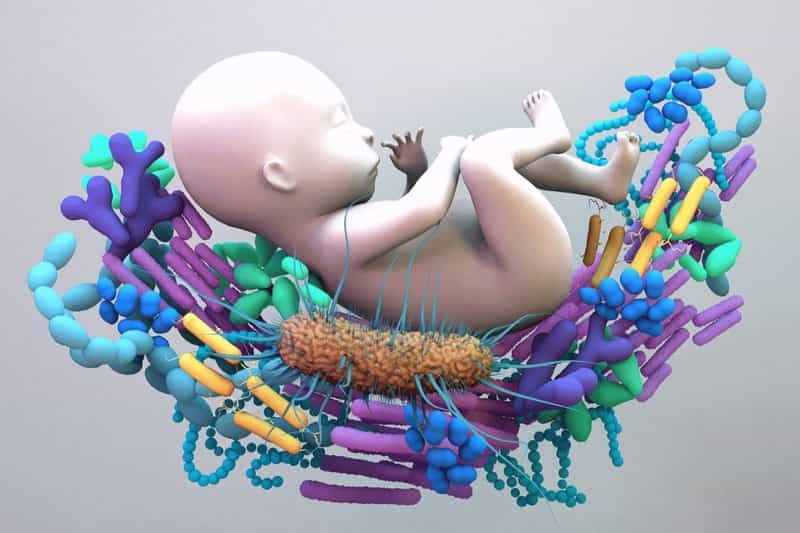
The human microbiome begins to develop at birth and continues to evolve throughout our lifetime. Here are some key stages in the development of the human microbiome:
Early colonization: During birth, newborns are colonized with bacteria from their mother’s birth canal and skin, as well as the surrounding environment. Breast milk also contains a variety of beneficial bacteria that can help to establish a healthy microbiome.
Infant gut microbiome: The gut microbiome of infants is initially dominated by bacteria from the Actinobacteria and Bifidobacterium families, which are believed to play an important role in infant digestion and immune system development.
Toddler gut microbiome: As toddlers begin to transition to solid foods, the diversity of their gut microbiome increases, with the introduction of new bacterial species that help to break down more complex carbohydrates and fiber.
Adult microbiome: By adulthood, the gut microbiome has stabilized to a certain extent, although it can still be influenced by factors such as diet, medication use, and lifestyle factors such as stress and exercise.
Aging and the microbiome: As we age, the composition of the microbiome may change, with a decrease in beneficial bacteria and an increase in potentially harmful species. This can be influenced by factors such as diet, medication use, and changes in the immune system.
Overall, the development of the human microbiome is shaped by a complex interplay between genetics, environmental factors, and the host’s immune system. Understanding how the microbiome develops and evolves over time is an important area of research, with potential implications for the prevention and treatment of a range of diseases.
Functions of Human Microbiome
Role of Microbiome in human health and Diseases
The microbiome plays a critical role in human health and disease, influencing a wide range of physiological processes and contributing to the development and progression of various diseases.
Here are some key ways in which the microbiome impacts human health:
Digestive health: The microbiome is essential for maintaining a healthy digestive system, helping to break down and absorb nutrients from food, and protecting against harmful pathogens.
Immune function: The microbiome is closely linked to immune function, with certain bacterial species helping to regulate immune responses and protect against infections.
Metabolic health: The microbiome plays a role in regulating metabolism and energy balance, with disruptions to the microbiome linked to conditions such as obesity and type 2 diabetes.
Mental health: The microbiome has been linked to various aspects of mental health, including mood disorders such as depression and anxiety.
Skin health: The microbiome also plays a role in maintaining healthy skin, with disruptions to the skin microbiome linked to conditions such as acne and eczema.
However, disruptions to the microbiome can also contribute to the development and progression of various diseases. For example:
Inflammatory bowel disease (IBD): IBD is a group of disorders characterized by chronic inflammation of the digestive tract. Disruptions to the gut microbiome have been linked to the development and progression of IBD.
Autoimmune diseases: The microbiome has been implicated in the development of various autoimmune diseases, such as rheumatoid arthritis and multiple sclerosis.
Allergies and asthma: The microbiome have been linked to the development of allergies and asthma, with disruptions to the gut microbiome in early life thought to increase the risk of these conditions.
Cancer: The microbiome has been implicated in the development and progression of various types of cancer, including colorectal cancer.
Overall, the role of the microbiome in human health and disease is a rapidly evolving area of research, with potential implications for the prevention and treatment of a wide range of conditions.
Digestion and absorption of food
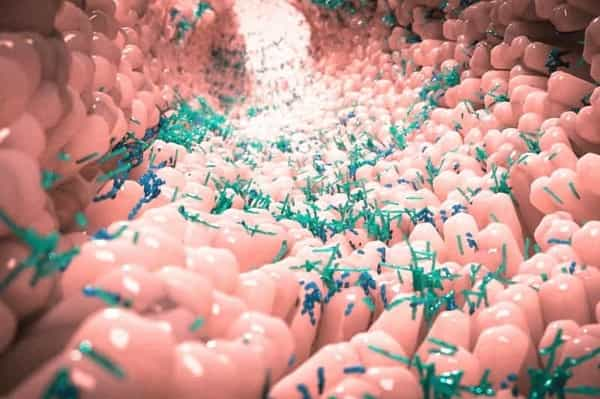
Digestion and absorption of food is a complex process that involves multiple organs and the microbiome in the gastrointestinal tract.
Here’s a brief overview of the steps involved:
Mouth: The digestion of food begins in the mouth, where enzymes in saliva begin to break down carbohydrates.
Esophagus: Once the food is swallowed, it travels down the esophagus and into the stomach.
Stomach: In the stomach, food is further broken down by stomach acid and enzymes, and converted into a liquid called chyme.
Small intestine: The majority of nutrient absorption occurs in the small intestine. Enzymes from the pancreas and bile from the liver help to break down carbohydrates, proteins, and fats, and transport them across the intestinal lining and into the bloodstream.
Large intestine: The large intestine, or colon, is where water and electrolytes are absorbed from undigested food, and where the microbiome plays a critical role in the fermentation of certain fibers and the production of certain vitamins.
The microbiome in the gut also plays a crucial role in the digestion and absorption of food. Certain bacteria in the gut help to break down complex carbohydrates and fiber that the body cannot digest on its own, producing short-chain fatty acids that are used as an energy source by the body. The microbiome is also involved in the production of certain vitamins, such as vitamin K and B vitamins.
Disruptions to the microbiome, such as the use of antibiotics or changes in diet, can have a significant impact on the digestion and absorption of food and may contribute to conditions such as irritable bowel syndrome and inflammatory bowel disease. Maintaining a healthy and diverse microbiome through a balanced diet and lifestyle is important for optimal digestive function and overall health.
Protection against pathogens
The microbiome plays a critical role in protecting against pathogens, or disease-causing microorganisms, in several ways:
Competitive exclusion: The microbiome helps to prevent the colonization of harmful pathogens by occupying the same ecological niches. This is known as competitive exclusion, where the “good” bacteria out-compete the “bad” bacteria for nutrients and space in the gut.
Production of antimicrobial substances: Some bacteria in the microbiome produce antimicrobial substances such as bacteriocins, which are toxic to other bacteria and prevent their growth.
Immune modulation: The microbiome is closely linked to immune function, with certain bacterial species helping to regulate immune responses and protect against infections. The microbiome can also influence the development of the immune system, particularly in early life.
Maintaining the integrity of the gut barrier: The gut lining acts as a physical barrier between the microbiome and the rest of the body. The microbiome helps to maintain the integrity of the gut barrier by promoting the production of mucus and other protective substances that prevent harmful pathogens from entering the bloodstream.
Disruptions to the microbiome, can disrupt the balance of beneficial bacteria and make it easier for pathogens to colonize and cause infection. This can lead to conditions such as Clostridium difficile infection, which is caused by an overgrowth of harmful bacteria in the gut. Maintaining a healthy and diverse microbiome is therefore important for protecting against infections and maintaining overall health.
Development and regulation of the immune system
The development and regulation of the immune system are closely linked to the microbiome, particularly in early life.
Here’s how the microbiome plays a role:
Colonization during birth: During birth, the newborn is exposed to the mother’s microbiome, which helps to establish the baby’s own microbiome. Vaginal birth is particularly important in this regard, as the baby is exposed to the mother’s vaginal microbiome, which helps to colonize the baby’s gut with beneficial bacteria.
Breastfeeding: Breast milk contains numerous components that help to promote the growth of beneficial bacteria in the baby’s gut, and also provide immunological protection against pathogens.
Immune system development: The microbiome plays a critical role in the development of the immune system, particularly in early life. The presence of certain bacterial species helps to train the immune system to recognize and respond to potential pathogens, while also promoting immune tolerance to harmless substances.
Regulation of immune responses: The microbiome can also help to regulate immune responses, particularly in the gut. Certain bacterial species produce molecules that help to modulate immune responses and prevent inflammation.
Disruptions to the microbiome, such as the use of antibiotics or changes in diet, can have a significant impact on immune system development and regulation. This may contribute to the development of autoimmune diseases, allergies, and other immune-related conditions. Maintaining a healthy and diverse microbiome through a balanced diet and lifestyle is therefore important for optimal immune function and overall health.
The microbiome plays an important role in the production of vitamins and other metabolites, which are important for various biological processes.
Here are a few examples:
Vitamin synthesis: Certain bacterial species in the gut are able to synthesize vitamins that are essential for human health, including vitamin B12, vitamin K, and folic acid. These vitamins are involved in a wide range of biological processes, including DNA synthesis, energy metabolism, and blood clotting.
Short-chain fatty acids: The microbiome also produces short-chain fatty acids (SCFAs), which are produced through the fermentation of dietary fiber. SCFAs are important for maintaining gut health, as they help to nourish the cells that line the gut and promote the growth of beneficial bacteria.
Amino acids and neurotransmitters: The microbiome is also involved in the production of amino acids and neurotransmitters, which are important for various biological processes. For example, certain bacterial species produce gamma-aminobutyric acid (GABA), which is a neurotransmitter that has been linked to the regulation of mood and anxiety.
This can have significant implications for human health, as deficiencies in certain vitamins or other metabolites can lead to a range of health problems. Maintaining a healthy and diverse microbiome through a balanced diet and lifestyle is therefore important for optimal metabolic function and overall health.
Factors Affecting Human Microbiome
Diet and Nutrition
Diet and nutrition play a crucial role in shaping the composition and function of the human microbiome.
Here are a few ways in which diet can impact the microbiome:
Fiber: Fiber is an important nutrient that is essential for maintaining a healthy microbiome. Fiber is fermented by bacteria in the gut, which produces short-chain fatty acids (SCFAs) that are important for gut health. A diet that is low in fiber can lead to a reduction in the number and diversity of beneficial bacteria in the gut.
Macronutrients: The composition of macronutrients (carbohydrates, fats, and proteins) in the diet can also impact the microbiome. For example, diets that are high in saturated fat have been shown to alter the composition of the gut microbiome, potentially increasing the risk of metabolic diseases.
Phytochemicals: Phytochemicals are compounds that are found in plant-based foods and have been shown to have a range of health benefits. Some phytochemicals, such as polyphenols, have been shown to have prebiotic effects, promoting the growth of beneficial bacteria in the gut.
Probiotics and prebiotics: Probiotics are live bacteria that are consumed to provide health benefits, while prebiotics are non-digestible compounds that promote the growth of beneficial bacteria in the gut. Both probiotics and prebiotics can be consumed through diet or supplementation.
A balanced and varied diet that is rich in fiber, phytochemicals, and other essential nutrients is important for maintaining a healthy and diverse microbiome. Disruptions to the microbiome, such as the use of antibiotics or changes in diet, can impact overall health and increase the risk of certain diseases. By prioritizing a healthy diet and lifestyle, individuals can help to promote optimal gut health and overall well-being
Lifestyle and Environment
In addition to diet, lifestyle, and environment also play a crucial role in shaping the composition and function of the human microbiome.
Here are a few ways in which lifestyle and environment can impact the microbiome:
Exercise: Regular physical activity has been shown to promote the growth of beneficial bacteria in the gut. Exercise can also help to reduce inflammation in the body, which can have a positive impact on the microbiome.
Stress: Chronic stress has been shown to alter the composition of the gut microbiome, potentially increasing the risk of certain diseases. Strategies for managing stress, such as mindfulness meditation or yoga, may help to support a healthy microbiome.
Antibiotics: Antibiotics are designed to kill bacteria, but they can also impact the composition and diversity of the gut microbiome. Overuse of antibiotics can lead to the loss of beneficial bacteria in the gut and an increased risk of certain diseases.
Environmental toxins: Exposure to environmental toxins, such as pesticides or heavy metals, can also impact the microbiome. These toxins can alter the composition of the gut microbiome and potentially increase the risk of certain diseases.
Medications
Medications, particularly antibiotics, can have a significant impact on the composition and function of the human microbiome. Antibiotics are designed to kill bacteria, and while they are effective at treating bacterial infections, they can also have unintended consequences for the gut microbiome.
Here are a few ways in which medications can impact the microbiome:
Antibiotics: Antibiotics can lead to the loss of beneficial bacteria in the gut, potentially reducing microbial diversity and altering the composition of the microbiome. This disruption to the microbiome can lead to a range of negative health outcomes, including an increased risk of certain infections and metabolic disorders.
Other medications: Other medications, such as non-steroidal anti-inflammatory drugs (NSAIDs) and proton pump inhibitors (PPIs), have also been shown to impact the microbiome. NSAIDs can lead to intestinal permeability, which can impact the composition of the microbiome, while PPIs have been shown to alter the gut microbiome and increase the risk of certain infections.
Probiotics: Probiotics are live bacteria that can be consumed to provide health benefits. While antibiotics can disrupt the microbiome, probiotics may help to restore microbial diversity and promote the growth of beneficial bacteria in the gut.
Fecal microbiota transplantation (FMT): FMT is a medical procedure in which fecal matter from a healthy donor is transplanted into the gut of a patient. FMT has been shown to be effective at treating certain infections and diseases that are linked to disruptions in the gut microbiome.
Genetics
Genetics can also play a role in shaping the human microbiome. While the microbiome is largely influenced by environmental factors, such as diet and lifestyle, genetic variations can impact an individual’s susceptibility to certain diseases and conditions that are linked to disruptions in the microbiome.
Here are a few ways in which genetics can impact the microbiome:
Host genetics: Variations in an individual’s genes can impact their susceptibility to certain diseases that are linked to the microbiome, such as inflammatory bowel disease (IBD). Genetic variations can impact the production of immune system molecules that help to regulate the microbiome and maintain gut health.
Microbial genetics: The genetic makeup of the microorganisms that make up the microbiome can also impact their function and potential health benefits. For example, some strains of bacteria in the gut may produce beneficial metabolites, such as short-chain fatty acids, that can support gut health and overall well-being.
Host-microbe interactions: The relationship between an individual’s genetics and the microbiome is complex and involves numerous interactions between host genes and microbial genes. Certain genetic variations may impact the expression of genes that regulate the microbiome, potentially leading to disruptions in gut health and an increased risk of disease.
While genetics can play a role in shaping the microbiome, it is important to note that environmental factors, such as diet and lifestyle, are still the primary drivers of microbial diversity and composition in the gut. By prioritizing healthy habits, individuals can help to support a healthy and diverse microbiome, regardless of their genetic makeup.
Human Microbiome and Diseases
Microbial imbalance and diseases
Microbial imbalance, also known as dysbiosis, in the human microbiome, has been linked to a wide range of diseases and health conditions. Dysbiosis can occur when the composition and function of the microbiome are disrupted, potentially leading to an overgrowth of harmful microorganisms and a decrease in beneficial bacteria.
Here are a few ways in which microbial imbalance can contribute to the development of diseases:
Inflammation: Dysbiosis has been linked to increased levels of inflammation in the gut and throughout the body. This inflammation can contribute to the development of chronic conditions, such as inflammatory bowel disease (IBD), diabetes, and heart disease.
Infections: Dysbiosis can increase an individual’s susceptibility to infections, particularly those caused by harmful bacteria, such as Clostridium difficile (C. diff). This can lead to recurrent infections and may require antibiotic treatment to resolve.
Type 2 diabetes: Dysbiosis has also been linked to an increased risk of type 2 diabetes, with changes in the microbiome observed in individuals with the condition. It is thought that dysbiosis may lead to inflammation and insulin resistance, contributing to the development of diabetes.
Autoimmune diseases: Autoimmune diseases, such as rheumatoid arthritis and multiple sclerosis, have also been associated with dysbiosis. It is thought that dysbiosis may lead to increased intestinal permeability, allowing harmful substances to enter the bloodstream and trigger an immune response.
Obesity: The gut microbiome has been linked to the regulation of metabolism and energy balance in the body. Dysbiosis may contribute to the development of obesity by promoting the growth of bacteria that are associated with increased calorie absorption and fat storage.
Mental health: The gut-brain axis is a bidirectional communication pathway between the gut and the brain that involves the microbiome. Dysbiosis has been linked to changes in brain function and mental health, including depression, anxiety, and autism.
Overall, maintaining a healthy and diverse microbiome is important for overall health and well-being. By prioritizing healthy habits, such as eating a balanced diet, getting regular exercise, and minimizing unnecessary medication use, individuals can help to support a healthy and balanced microbiome.
Impact of Antibiotics on Microbiome
Antibiotics are a class of medications that are used to treat bacterial infections. While they can be life-saving in many cases, antibiotics can also have a significant impact on the human microbiome.
Here are a few ways in which antibiotics can affect the microbiome:
Disruption of microbial diversity: Antibiotics work by killing or inhibiting the growth of bacteria, which can lead to a decrease in the overall diversity of the microbiome. This can create an environment that is more conducive to the growth of harmful bacteria, potentially leading to dysbiosis.
Overgrowth of harmful bacteria: In addition to reducing microbial diversity, antibiotics can also lead to an overgrowth of harmful bacteria, such as Clostridium difficile (C. diff). This can lead to recurrent infections and may require additional antibiotic treatment to resolve.
Reduced production of beneficial metabolites: Some bacteria in the gut are responsible for producing beneficial metabolites, such as short-chain fatty acids (SCFAs), that are important for gut health. Antibiotics can reduce the production of these metabolites, potentially leading to a decrease in gut health.
Increased risk of diseases: Dysbiosis caused by antibiotics has been linked to an increased risk of a variety of diseases and conditions, including obesity, diabetes, and inflammatory bowel disease (IBD).
It is important to note that while antibiotics can have a significant impact on the microbiome, they are still an important tool in the treatment of bacterial infections. However, it is important to use antibiotics only when necessary and to take steps to support a healthy and diverse microbiome, such as eating a balanced diet and minimizing unnecessary antibiotic use.
Additionally, probiotics and other microbiome-targeted therapies may be beneficial in restoring a healthy microbiome after antibiotic treatment.
Emerging role of Microbiome in the development of diseases
The human microbiome has emerged as a significant player in the development of a range of diseases, beyond those traditionally thought of as being related to the gut or immune system. Recent research has revealed that the microbiome plays a crucial role in many aspects of human health, including metabolism, inflammation, and even brain function.
Here are a few examples of the emerging role of the microbiome in the development of diseases:
Cardiovascular disease: Recent studies have suggested that the microbiome may play a role in the development of cardiovascular disease. Dysbiosis has been associated with the development of atherosclerosis, a condition in which the arteries become clogged with fatty deposits, as well as hypertension.
Related Article: TOP CARDIOVASCULAR DISEASES AND HOW TO TREAT THEM
Neurodegenerative diseases: The microbiome has also been linked to the development of neurodegenerative diseases, such as Parkinson’s disease and Alzheimer’s disease. Dysbiosis has been observed in individuals with these conditions, and it is thought that the gut-brain axis may play a role in their development.
Human Microbiome and Therapeutics

Probiotics and prebiotics
The human microbiome has been found to play a critical role in many aspects of human health, including digestion, immune function, and disease prevention. As a result, researchers are exploring the potential of using the microbiome as a target for therapeutic interventions, including the use of probiotics and prebiotics.
Probiotics are live microorganisms, usually bacteria, that are believed to provide health benefits when consumed in adequate amounts. Probiotics are available in a range of forms, including supplements and fermented foods such as yogurt, kefir, and sauerkraut. Some strains of probiotic bacteria have been shown to improve digestive health, boost the immune system, and reduce inflammation. Additionally, probiotics have been associated with improvements in conditions such as irritable bowel syndrome, diarrhea, and eczema.
Prebiotics, on the other hand, are non-digestible food components that selectively stimulate the growth and/or activity of beneficial microorganisms in the gut. Foods that are high in prebiotics include asparagus, garlic, onions, bananas, and whole grains. Some prebiotic supplements are also available. Research has suggested that prebiotics may improve digestive health, reduce inflammation, and support the immune system. Additionally, prebiotics may have a positive impact on satiety and weight management.
There is growing interest in using probiotics and prebiotics as therapeutic interventions for a range of health conditions, including inflammatory bowel disease, obesity, and depression. However, the effects of probiotics and prebiotics on the microbiome can vary depending on factors such as the type and dose of the supplement, as well as an individual’s microbiome composition and overall health. Therefore, it is always advisable to consult with a healthcare professional before adding any supplements to your diet.
In addition to probiotics and prebiotics, other approaches to targeting the microbiome for therapeutic purposes include fecal microbiota transplantation (FMT), which involves the transfer of fecal material from a healthy donor into the gut of a patient, and the use of antibiotics to selectively target harmful bacteria in the gut. However, these approaches also come with risks and limitations, and more research is needed to fully understand their potential benefits and risks.
Fecal Microbiota Transplantation
Fecal microbiota transplantation (FMT) is a procedure in which fecal matter from a healthy donor is transferred to the gastrointestinal tract of a recipient in order to treat a variety of conditions related to microbial dysbiosis.
FMT has been used successfully to treat recurrent Clostridioides difficile infection (CDI), a condition in which the gut microbiota is disrupted and can lead to severe diarrhea and other symptoms. By introducing healthy microbiota from a donor, FMT can restore the balance of bacteria in the gut and alleviate symptoms of CDI.
Research has also shown potential for FMT to treat other conditions related to microbial dysbiosis, such as inflammatory bowel disease (IBD), irritable bowel syndrome (IBS), and even neurological disorders such as Parkinson’s disease.
Related Article: Parkinson’s Disease: Symptoms, Causes and Latest Updates
However, FMT is not without risks. In rare cases, the transfer of fecal matter from an unhealthy donor can introduce harmful pathogens or lead to other complications. Therefore, it is important for FMT to be performed under controlled conditions, with careful screening of donors and recipients.
In addition to safety concerns, FMT also raises ethical and regulatory questions. The use of fecal material as a medical treatment is a relatively new and untested practice, and there are still many questions about its long-term safety and effectiveness.
Overall, while FMT shows promise as a potential treatment for a range of conditions related to the microbiome, more research is needed to fully understand its potential benefits and risks and to develop safe and effective protocols for its use.
Future Directions in Human Microbiome Research

Emerging Research Areas
As research on the human microbiome continues to advance, new areas of investigation are emerging that have the potential to expand our understanding of the role that the microbiome plays in human health and disease.
Here are some emerging research areas:
Microbiome and brain function: Recent studies have suggested that the gut microbiome may play a role in brain function and behavior. Researchers are investigating the ways in which the microbiome may influence conditions such as depression, anxiety, and autism spectrum disorder.
Microbiome and cancer: There is growing evidence that the gut microbiome may play a role in the development of certain types of cancer, such as colorectal cancer. Researchers are investigating the mechanisms by which the microbiome may contribute to cancer development and exploring the potential of microbiome-based therapies for cancer treatment.
Microbiome and metabolic disorders: The gut microbiome has been implicated in the development of metabolic disorders such as obesity and type 2 diabetes. Researchers are investigating the ways in which the microbiome may influence metabolism and developing interventions that target the microbiome for the treatment of these conditions.
Microbiome and aging: There is evidence that the microbiome changes as we age, and that these changes may contribute to age-related health conditions. Researchers are investigating the mechanisms behind these changes and exploring interventions that may help to maintain a healthy microbiome throughout the aging process.
Microbiome and personalized medicine: As our understanding of the microbiome grows, there is potential for microbiome-based interventions to be tailored to individual patients based on their specific microbiome composition. Researchers are exploring the development of personalized microbiome-based therapies that could be used to treat a wide range of conditions.
Overall, the emerging research areas in the microbiome field are broad and diverse and hold significant potential for improving our understanding of the role that the microbiome plays in human health and disease.
Advances in Sequencing Technology
Advances in sequencing technology have revolutionized the field of microbiome research. Traditional methods of identifying microorganisms in a sample, such as culturing them in a laboratory, were limited in their ability to capture the full diversity of the microbiome. With the advent of high-throughput sequencing technologies, it is now possible to identify and characterize the entire microbial community present in a sample.
There are two main sequencing approaches used in microbiome research: amplicon sequencing and shotgun metagenomic sequencing. Amplicon sequencing targets a specific gene or region of the microbial genome, such as the 16S rRNA gene, and amplifies it for sequencing. This approach allows for a broad survey of the microbial community but provides limited information on the functional capabilities of the microbiome.
Shotgun metagenomic sequencing, on the other hand, sequences all the DNA present in a sample, including both microbial and human DNA. This approach allows for a more detailed characterization of the microbiome, including information on the functional capabilities of the microorganisms present.
Recent advances in sequencing technology have made these approaches faster, more accurate, and more cost-effective. For example, the development of long-read sequencing technologies has improved the accuracy and completeness of genome assemblies, allowing for more accurate characterization of individual microorganisms within the microbiome. Additionally, improvements in bioinformatics tools for analyzing sequencing data have enabled researchers to more accurately identify and classify microorganisms, as well as to better understand the functional capabilities of the microbiome.
Overall, advances in sequencing technology have greatly expanded our ability to study the human microbiome, and have paved the way for new insights into the role that the microbiome plays in human health and disease.
Personalized medicine and microbiome research
Personalized medicine is a rapidly growing field that seeks to tailor medical treatments to the individual patient based on their unique genetic, environmental, and lifestyle factors. Microbiome research has the potential to play a key role in personalized medicine by providing insights into the microbial communities that inhabit each individual’s body.
One area where microbiome research is already showing promise in personalized medicine is in the treatment of certain diseases. For example, researchers are exploring the use of fecal microbiota transplantation (FMT) as a treatment for conditions such as Clostridium difficile infection and inflammatory bowel disease. FMT involves transferring fecal material from a healthy donor to the patient’s gut, in order to restore a healthy microbial community and improve disease outcomes.
Another potential application of microbiome research in personalized medicine is in the development of microbiome-based diagnostic tools. By analyzing the microbial communities present in a patient’s body, researchers may be able to identify biomarkers that are associated with specific diseases. This could allow for earlier and more accurate diagnosis of these diseases, and could potentially lead to more targeted treatments.
In addition, microbiome research may also provide insights into how an individual’s microbiome interacts with medications. For example, certain medications may have different effects on the microbiome depending on the individual’s microbial community. Understanding these interactions could help to optimize medication dosages and minimize adverse effects.
Overall, personalized medicine and microbiome research are rapidly evolving fields, and there is still much to be learned about the complex interactions between the human body and its microbial inhabitants. However, the potential benefits of this research are significant and may lead to more effective and personalized treatments for a wide range of diseases.
